Before my breast cancer journey began, I might have guessed that a receptor is a mechanical part of a TV tower. Or something like that. Perhaps I wasn’t paying attention in Biology classes. (Sorry Mr. Bailey! But thanks for the quilt!)

What are Receptors?
Turns out receptors are a big deal when it comes to breast cancer. There are three types of receptors on a breast cancer cell:
- estrogen receptors
- progesterone receptors
- HER2 receptors (human epidural growth factor receptor 2)

What does it mean?
When you have breast tissue removed and sent to the lab, they identify whether or not the 3 receptors are positive or negative:
POSITIVE: This means that the cancer cell IS receiving signals from that hormone or protein, telling the cell to grow.
NEGATIVE: The cancer cell IS NOT receiving signals from that hormone or protein to grow.
Why is this important?
It determines your treatment. If any of the receptors come back Positive, then you are a candidate for “targeted therapy” – treatments that target specific characteristics of cancer cells. Good thing. Because other therapies like chemotherapy is a systemic therapy that targets all quickly growing cells … such as those that are in your gut, mouth, vagina, and that grow hair and nails. Yes, vagina.
So, for example, if you test positive for one of the two hormone receptors, then you can use hormone therapy to cut off the supply of estrogen and / or progesterone to the cells. These are called targeted therapies. Boom! Dead cancer cells without the need to throw a ton of chemotherapy at your body. (Note: This is when a positive result is actually positive … not like my last post when a Negative is a Positive.)
With that in mind, a triple negative pathology is NASTY … since only chemotherapy can be used.
What’s my pathology?
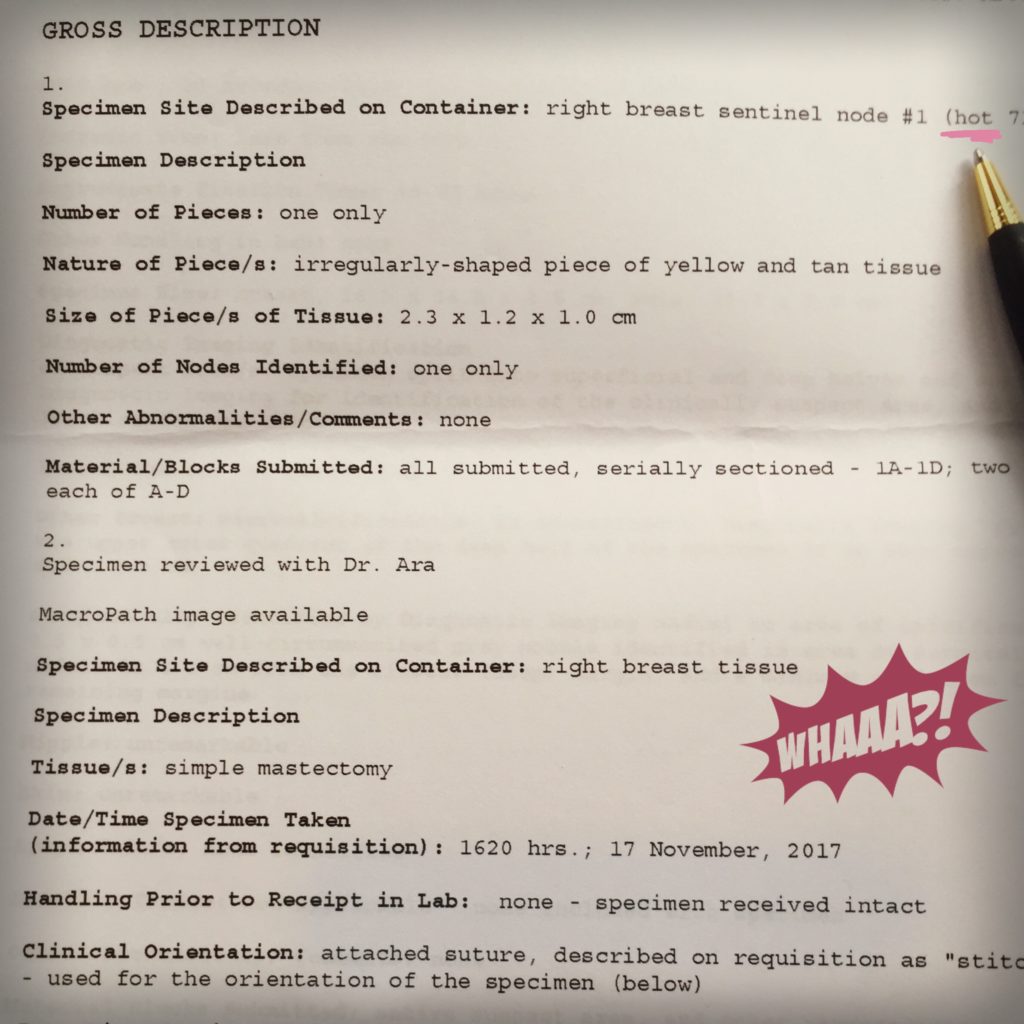
Let’s take a look (this is the 2nd path report btw):

My hormone receptors are both negative – so no hormone therapy for me. Move on to the HER2 receptors. Positive. WOOT WOOT!
What’s HER2?
HER2 are proteins that control how a healthy breast cell grows – until they stop working properly, get out of control and replicate in a crazy ass way.
This is the first thing I read about HER2, from the American Cancer Society website:
“For about 1 in 5 women with breast cancer, the cancer cells have too much of a growth-promoting protein known as HER2/neu (or just HER2) on their surface. These cancers, known as HER2-positive breast cancers, tend to grow and spread more aggressively. ”
Oh great. That doesn’t sound so positive…
So what’s next?
So to be sure that there there are no rogue cells journeying around my body, we have to hit those HER2 positive cancer cells with some drugs. And the best treatment is to combine some of the targeted therapy (good) with some of the systemic therapy (not as good). This is what my oncologist has recommended:
1. Herceptin (this is the brand name – the medical name, trastuzumab, is hard to say):
- This is a monoclonal antibody (a man-made immune system protein).
- It blocks the ability of the cancer cells to receive chemical signals that tell the cells to grow.
- Sometimes it is given alone and sometimes accompanied with chemotherapy.
- Causes flu like side effects (fever, chills, nausea, muscle aches).
- Oh, and it can cause congestive heart failure … more on that in another blog post…
2. Taxol (chemical name Paclitaxel)
- One of the taxane chemotherapies that interfere with the cell’s ability to divide.
- In order for it to find the cancer cells it needs to hitch a ride on herceptin, which incredibly knows where to go (because it’s targeted …. remember?).
- It uses solvents to dissolve paclitaxel, the main ingredient, so the medicine can enter the bloodstream. I will have to take pre-medications to minimize reactions to the solvents. Oh can’t wait for that.
So that’s where we’re at folks!! I know what’s coming … just have to firm up a few dates and get myself fitted with a portacath!
Oh so many more stories to come… like what I’m going to do with this stunning hair before I lose it all!!