A couple of weeks ago I finally got to meet the renowned plastic surgeon Dr. D, at his office in the dirty dirty Schwa, broken wrists and all (he’s not operating right now, relax). First time I’ve ever visited a doctor and shopped at Chapters in the same location, but whatever. Silver linings are everywhere, I find!

Dr. D
I arrived to a small waiting room that was empty save for two older Italian ladies who were struggling to understand the information page they had been assigned to complete. I asked if there was anyone there – they indicated in broken English that the receptionist was out for a coffee. Huh? Within moments Dr. D himself emerged and handed me my own clipboard, then 5 minutes or so later he re-emerged and got me. Not typical waiting room protocol, but oh well!!
Armed with my notepad and pen, I followed him into a small office – typical 2 chairs in front of a desk, atypical large reclining type exam chair (like a dentist’s chair) in the corner. Weird. But ok. Maybe boob exams need to be upright to observe perkiness. (My mind works this way.)
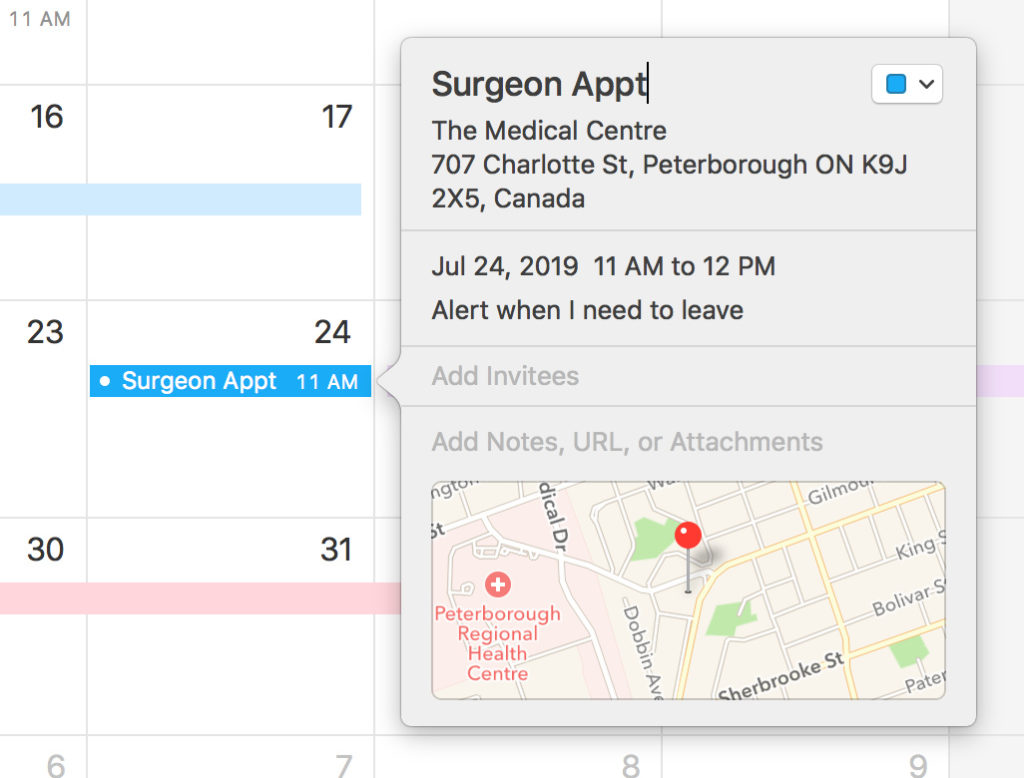
He thanked me for coming, I asked him how his wrists were healing up – small talk kind of thing, and then he asked me lots of questions – when was my bilateral mastectomy, had I had any operations other than that, etc. He had never heard of a SCAD heart attack – I explained it – he indicated that I’d have to be cleared for any surgery by my cardiologist. Interesting fact #1.
Once he was done asking background questions he opened a drawer and pulled out two sample boobs. This is where I leaned forward in my chair.
The boobies
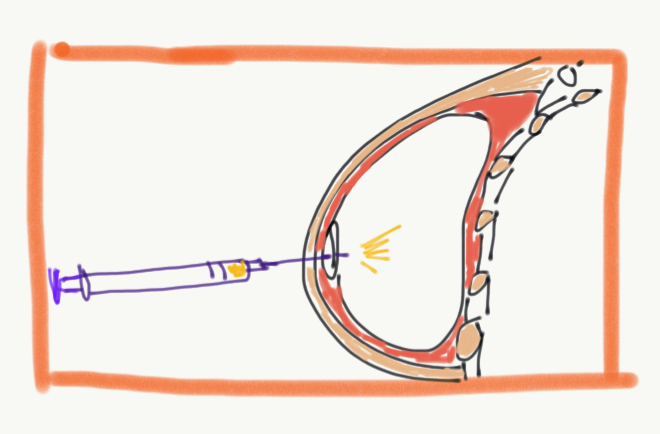
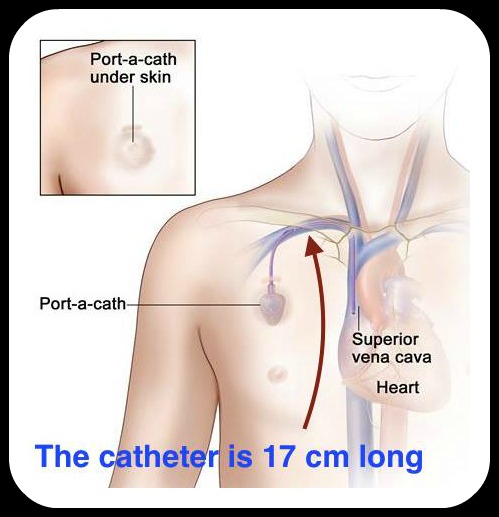
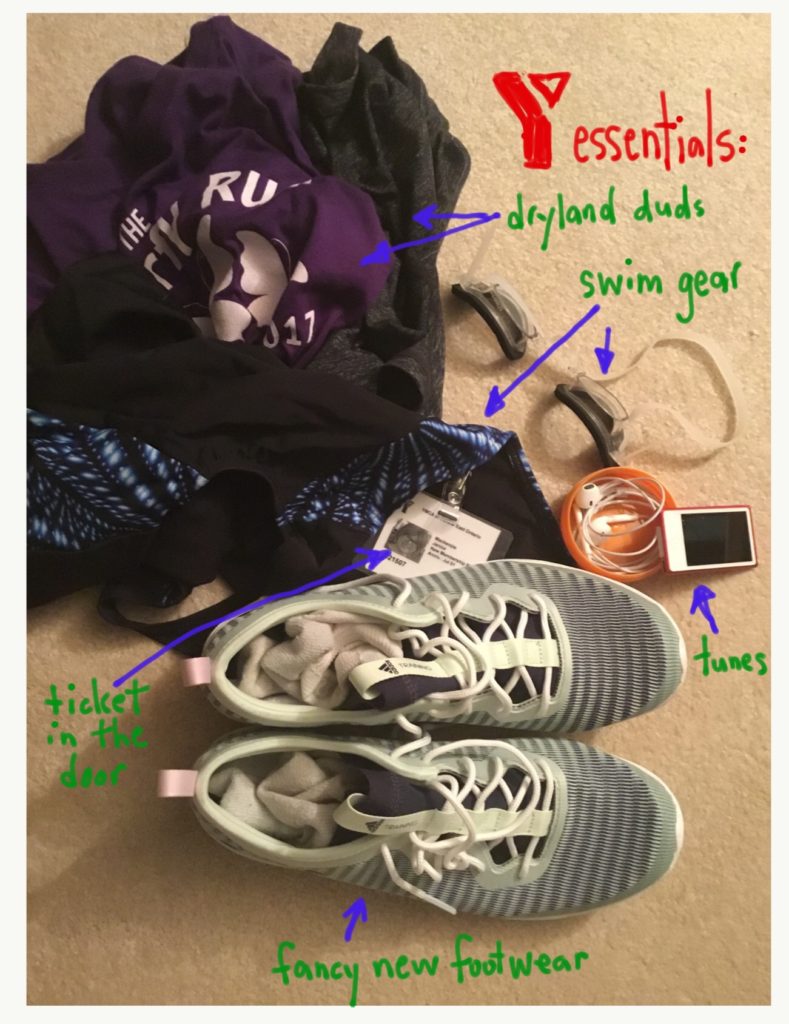
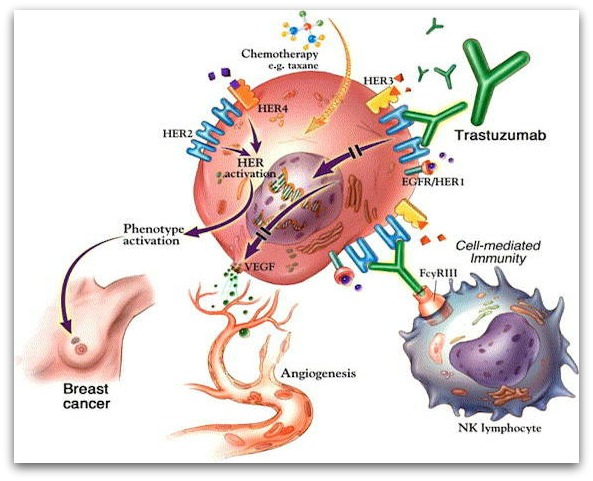
He started by showing me a sample of the expander boob (proper term is tissue expander) and explained that after an incision is made across the scar line, the expander is placed behind the pectoral muscle. Saline is injected once a week for 5 weeks (or until the desired size is reached). The expander has a round spot on the top that is made of a different material – the injection goes in there. But I didn’t ask about any more details. (Expander questions weren’t on my list lol.) If you are interested, you can look at what the Mayo Clinic has to say (a favorite resource of mine).
Then he chose a suitable implant, noting my previous bra size and commented “you have more droop to your skin” (um, ok … I know what you are getting at and I’m 54, ok?). He handed it to me. Of course I stuck it against my chest and thought to myself “There is no fucking way I’m going to wear a bra again!” which translated to me explaining in the nicest way possible that I don’t actually want breasts – I just want things smoothed out. Can’t you do that?
Pause. Dead air kind of pause.
The “this is want I want, what I really really want” discussion
I suppose it’s not common for a patient to come to you and say that they don’t actually want what you have to offer (boobs). I told him ya, I really just want to smooth it all out. Is that possible? So then he said he had to take a look at my chest. He left while I put a robe on (likely because “take your shirt off so I can have a look” sounds inappropriate – but really, … I mean he’s just going to pull back the robe and look anyway! Waste of time. But it did allow me a moment to capture this stunning robe in a mirror photo.)

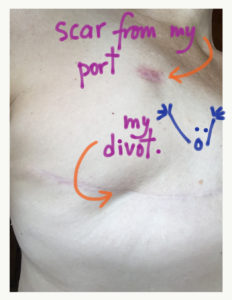
So I sat in the dentist’s chair and waited. He came in and asked me to stand up (so why have the chair?). He then looked at my chest, allowing me the opportunity to point out exactly what I want smoothed out. Isn’t it OBVIOUS? OMG.
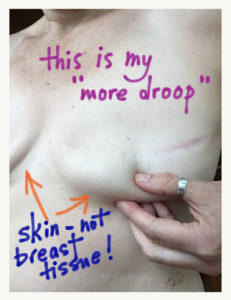
Here’s the first shocking info: when I grabbed onto the fatty remnants of boobie and said “Can’t you just get rid of this leftover breast tissue … I mean why is it even here?”, he told me that it’s not breast tissue. OK WHAT? Nope, it’s SKIN. (Well it’s skin that looks an awful lot like the bottom of my old boobs!!) Interesting fact #2. AND … if he removes it, it will be concave. Interesting fact #3.
I’m thinking that it would be like the divot that Dr E (initial surgeon) causally told me occurred because they likely took too much fat attached to the skin in that spot.
So then Dr. D gave me a bit of an anatomy lesson – showed me where my pecs start and explained that the entire breast was removed. I said “so the breast is in a capsule?” – he confirmed that more or less, yes. Interesting fact #4 BUT I can’t seem to verify this with Dr. Google which bugs me. Regardless, all this time I thought they just missed some of my boobs.
Dr. D went back to the implant drawer and grabbed another sample – a considerably flatter implant with a much greater diameter. He said that this implant would achieve the effect that I want. That is, if I want an implant.

But … do I want an implant?
No I really don’t. I don’t want to have a foreign body in me if I don’t HAVE to. “Lots of people have foreign bodies in them and are fine.” Dr. D had noted. True. Prosthetic hips and knees, pins and bolts to hold together plates that support broken bones, stents, pacemakers… But breasts are optional. Cosmetic. Other implants are not.
At the beginning of our meeting he said (with resignation in his voice) “I’m sure you’ve heard about the recall of textured tissue expanders and implants in the news.” Yes, I said, I had. (I can’t imagine that women getting cancer from a specific type of implants is particularly good for business.) He explained that implants are made of silicone. I listened. And I asked if there are other options.
Dr. D’s Wife
It turns out that Dr. D’s wife is also a surgeon who specializes in reconstruction using the DIEP Flap method. (Two breast people. Imagine what that means, just for a moment.) I’d seen this term referenced here and there but didn’t know a lot about it. Dr. D gave me a summary: fat is moved from one part of your body to recreate your breast. But before he’d explain further, he needed to know if I am a candidate – in other words, do I have enough fat to move. (I was literally scoffing out loud at this point – OMFG my belly might be an ASSET!! I’m the IDEAL candidate! Interesting fact #5.)
He asked me to unzip my pants so he could have a look at my belly (no robe required here, I noted). And then to drop the robe off my shoulders so he could see my back fat (the reason I won’t try on sports bras at LuLu Lemon anymore). He pronounced me a candidate DUH and we sat back down and he told me:
- it is a day long surgery (really, a day? You mean 24 hours? 5 hours? Come on. I’m a details person. But I let it go.)
- an incision is made across the belly (right across …)
- tissue and a bit of your abdominal muscles are removed (my FAT and a blood supply source)
- implant is done
- the blood supply has to be carefully connected so that the tissue does not necrotize (um gross)
- you have to stay in the H for approx 3 days
- your abs take a while to heal
I asked if chunks are taken out of the belly – how does that work (imagining two hunks of fat taken out). “No, it’s an incision across … like a tummy tuck.” OK ARE YOU SERIOUS RIGHT NOW?? (Obviously Interesting fact #6, am I right?)
He then showed me what the two procedures look like when they are healed – implant versus DIEP Flap. Essentially implants are more perky and symmetrical and there is a massive abdominal scar with the DIEP Flap. There are plenty of stories of people who have had the DIEP flap surgery done – this one is a good one to look at!
Risks
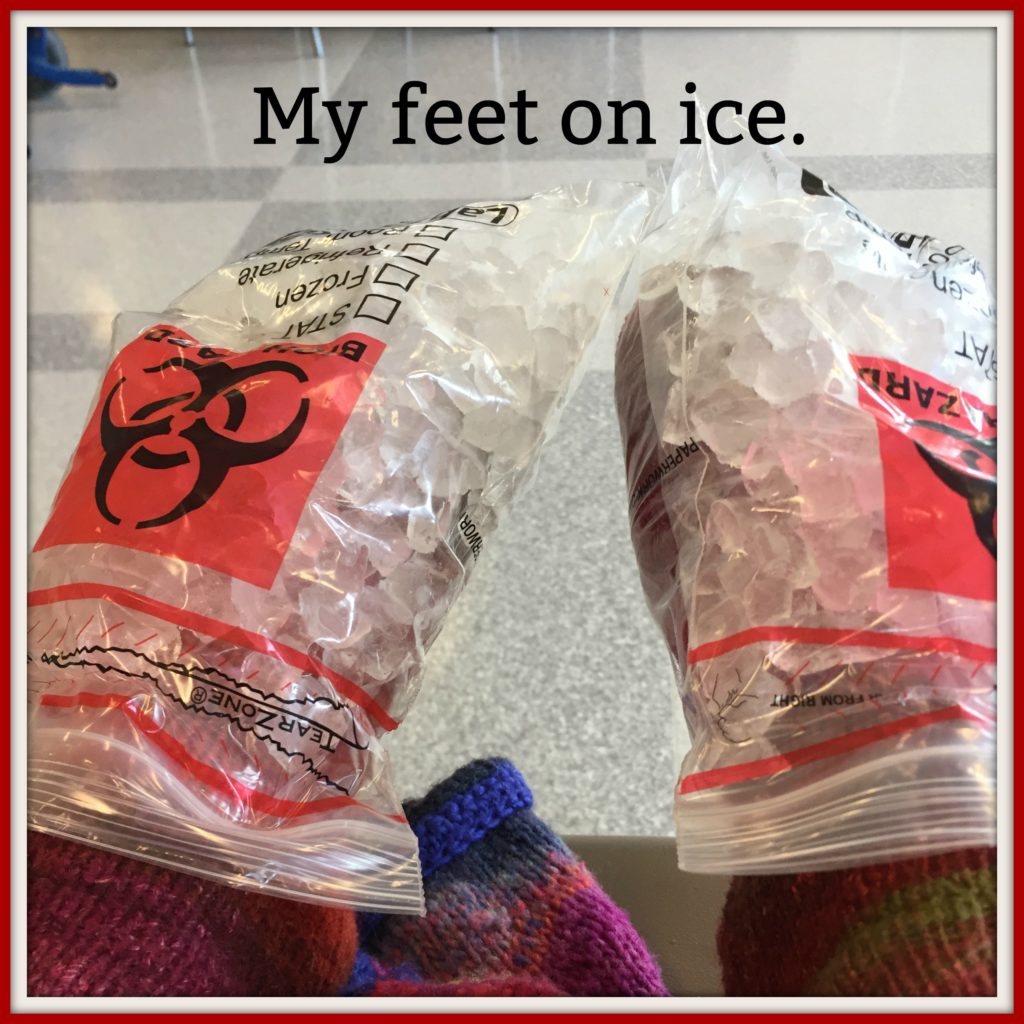
I asked about infection and risks (thanks Jenny). He admitted that yes, implant surgery comes with a much higher risk of infection. “It’s a foreign body.” (Calmly stated, like I’m an idiot.) Note that he did NOT talk about any other risks. But I will tell you!
I follow #flatandfabulous on Instagram – a hashtag used by cancer survivors who have had a unilateral or bilateral mastectomy (one or two boobies removed). There are many interesting, brave, strong women who share their photos, stories, challenges, fears, etc on instagram. Recently I started following @hollykthrasher who had implants removed after they made her very sick. It’s called an EXPLANT. Interesting fact #7.
Coles notes: Holly went through implant surgery, had marvelous tattoos done and yet was never feeling well afterwards (heart palpitations, sinus issues, muscle & joint pain, chronic inflammation, insomnia). She finally determined, through intrepid research, that her implants were making her sick. She had them removed. Here they are (with the skin and part of her tattoos clinging on).

Note: these implants were in Holly for almost 3 years. You can see a layer of tissue around the implants. These “capsules” are formed by the body as a response to the foreign body being there – likely as a matter of protection. Explant surgery is painful and difficult, since the capsule must be removed as well.
Second Note: Within weeks after the explant surgery Holly said she felt like her old self. You can read more about her or buy a copy of her book (that chronicles her journey) on her blog.
Of course this is not to say that everyone will develop “Breast Implant Illness” (BII is a thing!). But some do.
What’s Next?
I’m going to see Dr. D’s wife, at Sunnybrook and find out more about the DIEP Flap surgery. (We’ll call her Dr. S.) I don’t know that I want the procedure done, but I don’t want to say no till I have all of the information. I have to admit, the tummy tuck / smooth chest combo pack is rather appealing.
I can feel a pros and cons list forming.




















 I had my head shaved last week, on week 9 of chemo. (My hair actually lasted a LONG time!) I had it shaved since it was looking a bit Donald Trumpish. It really did look pretty horrible – my scalp was very visible and the remaining hair was wispy and elfin. I could stand it up and look like a troll. (kind of fun…) And my wigs would just float around on top of my head. (very irritating) So I went with the kids to Jenny’s shop in Lakefield and we all had haircuts.
I had my head shaved last week, on week 9 of chemo. (My hair actually lasted a LONG time!) I had it shaved since it was looking a bit Donald Trumpish. It really did look pretty horrible – my scalp was very visible and the remaining hair was wispy and elfin. I could stand it up and look like a troll. (kind of fun…) And my wigs would just float around on top of my head. (very irritating) So I went with the kids to Jenny’s shop in Lakefield and we all had haircuts.