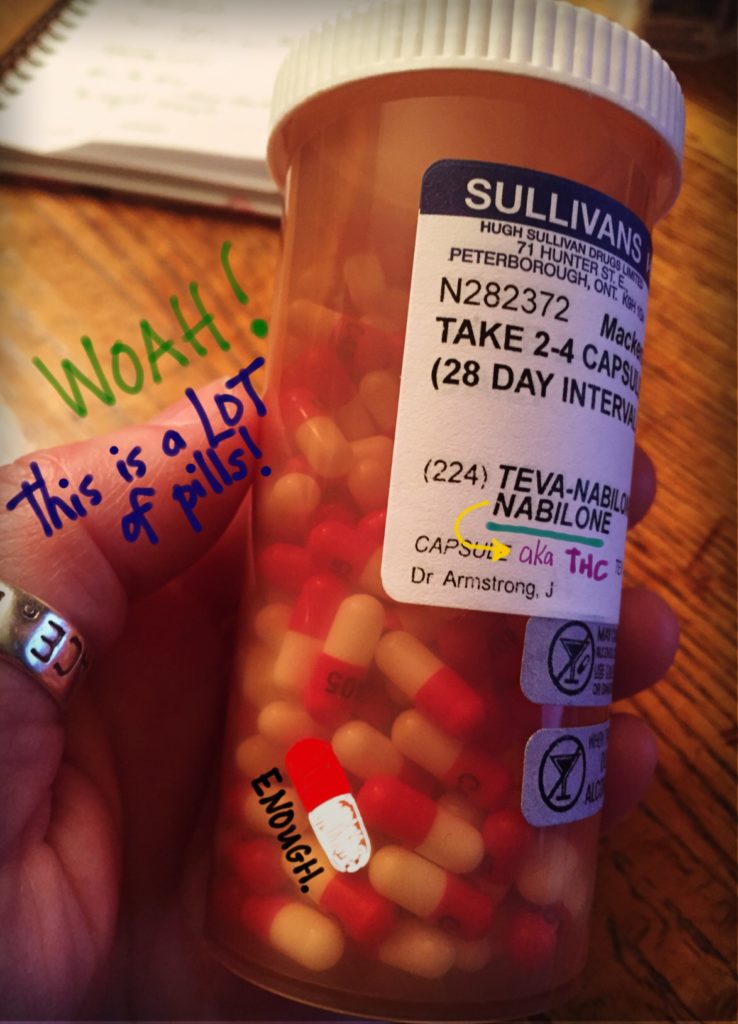
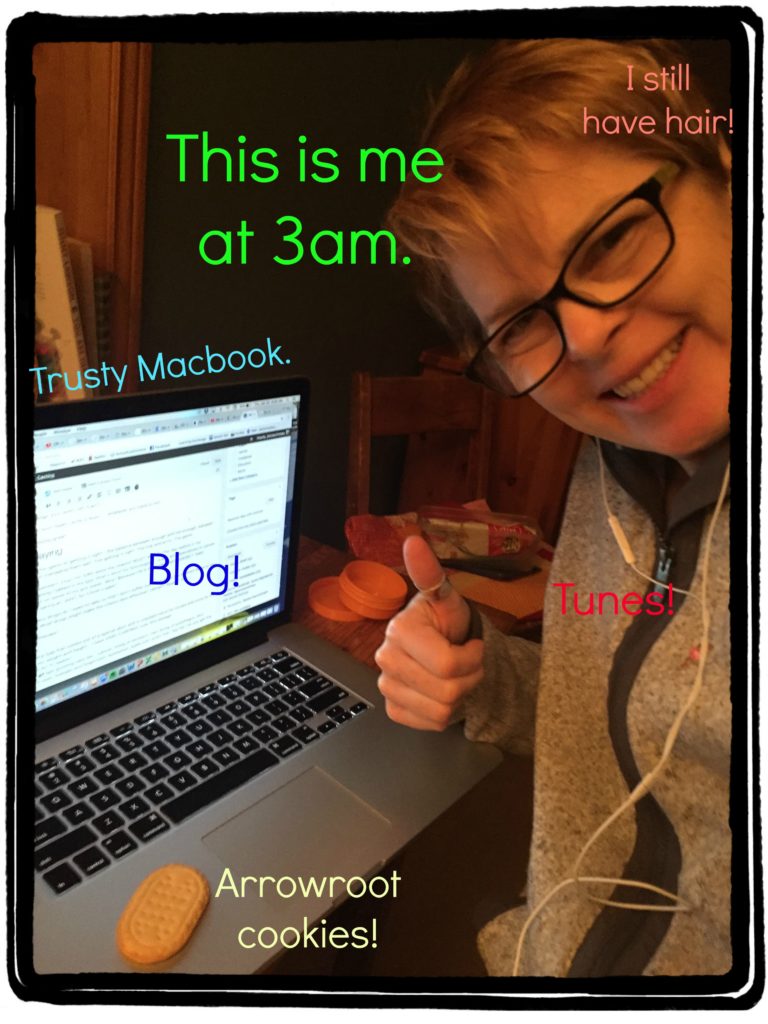
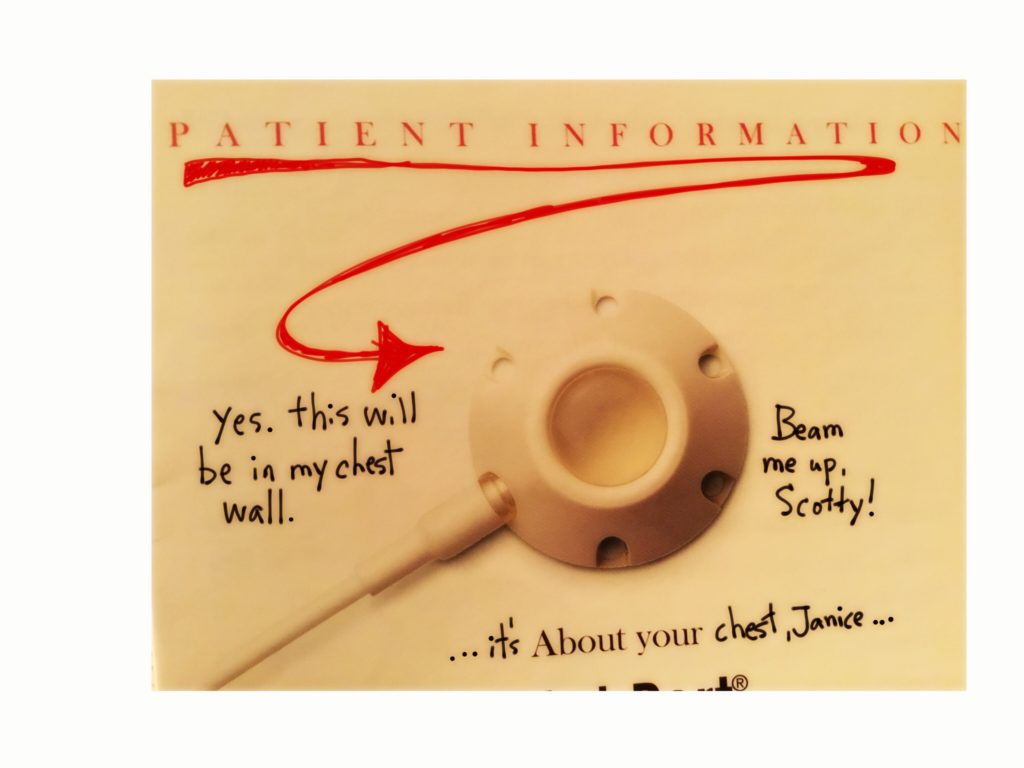
I’ve been done chemo for almost 3 months now. I feel great, I’m back at work half time, I’m pain free, I have some hair growth happening, I can drink wine and eat anything without repercussions. There are a few side effects that I still have to deal with from the drugs that I’m still taking: beta blockers (to keep my heart safe) and Herceptin (life saving breast cancer treatment). Mostly tiredness. Some aching. That kind of thing. Nothing horrific.
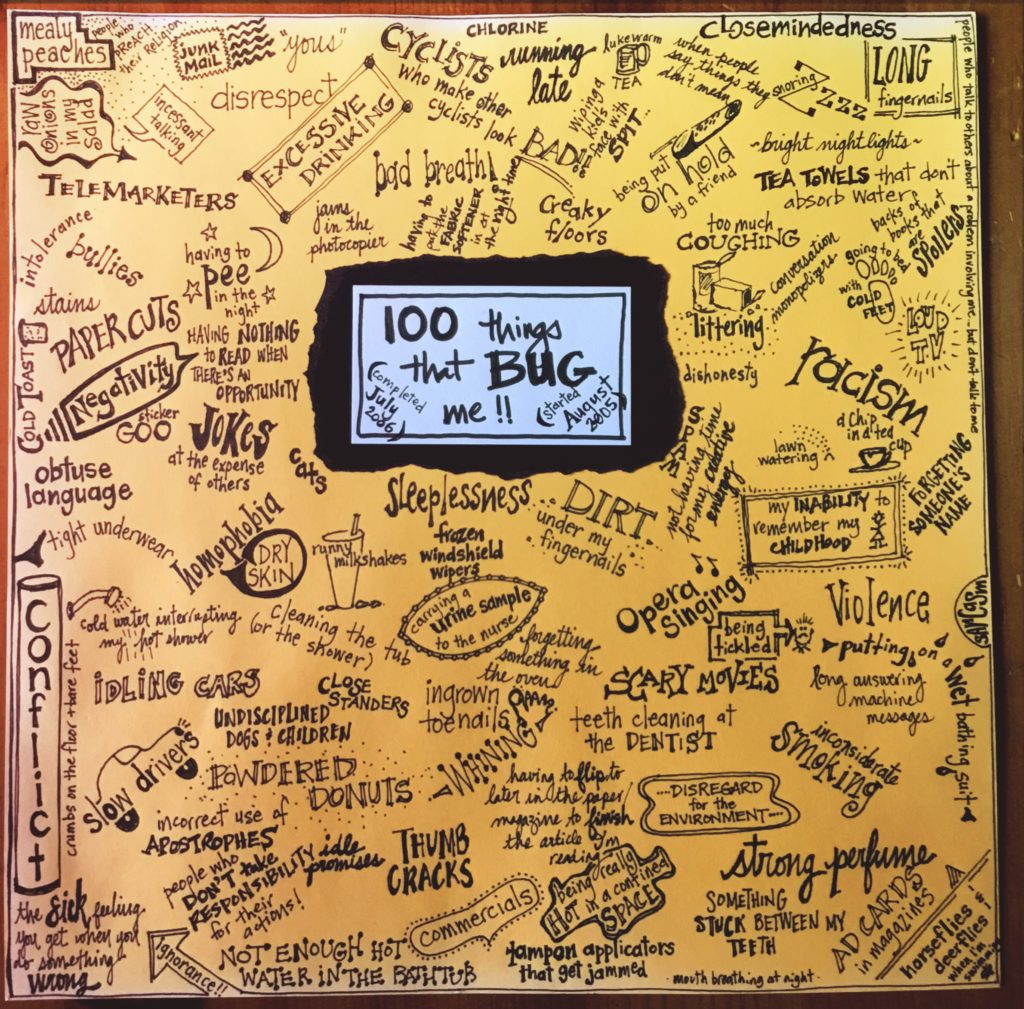
I do have one major side effect involving my brain. Basically it’s sluggish and really shitty at couple of its jobs. Most people in the field call it chemo brain. People laugh when you say that … or likely think “oh here she goes playing the cancer card …” (and maybe I did that in a few times, ok whatever). But it’s real, people!
Here’s a tutorial, but first:
How does memory even work?
In basic terms are three types of memory:
- sensory – outside of conscious control … has to do with the 5 senses and lasts less than a second (I’m not worried about this one!)
- short term – the ability to remember and process information at the same time (this is me glancing at my BP stats on the monitor and holding them in my head till I can open my journal and jot them down … if it takes too long I forget) – if I make a conscious effort to retain it (consolidation), then it will transfer into my long term memory through the hippocampus (who doesn’t love that word?)
- long term – storage of information over a long period of time – some researchers believe that humans can retain an endless amount of information (useless and otherwise), we just have a hard time accessing it (I find this hard to believe – no idea what passé compose is … although I remember the words passé compose. whatever.) – to make a long term memory you have to change or strengthen the neurons (nerve cells) in your brain – there is some evidence that if the connections between the neurons in a neural network are overwritten OR weakened / damaged you can forget. HA!

What is chemo brain, ACTUALLY?
The American Cancer Society defines it as a decrease in mental sharpness and an inability to concentrate and remember details.
Experts agree that there are memory loss issues related to having had cancer treatment, but they don’t attribute it all to the chemotherapy. After all, it could be any number of things that happen during treatment, namely:
- stress
- lack of sleep (some drugs cause insomnia while others, like steroids, make you feel like you’re on crack)
- poor nutrition (crackers, porridge and pudding … not a lot there but white glue substitutes)
- stress
- 100 other things that don’t apply to me, like radiation, pain, stem cell transplant, surgery (ok I had surgery but my brain seemed totally fine after that…)
I agree that lack of sleep and stress might affect my brain, and poor nutrition? This is questionable. University students eat crap for months on end and are getting degrees, so I don’t believe it. Plus, there is NO WAY that a massive amount of chemo poured into my superior vena cava wasn’t largely responsible for messing up my brain. I blame it on the drugs.
(This is your brain. This is your brain on drugs. Any questions?)
How is chemo brain affecting me?
My long term memory recall is tragically slow.
When I run into someone who I know but haven’t known for very long – like a colleague who works in another part of the board, I have to WORK HARD to pull the name out of my brain. It’s incredibly annoying. When this was first happening to me, in the first few minutes that we are chatting I was not listening AT ALL. I was still trying to remember their name. Don’t get me wrong, I’ve always been shit at learning names, but this is not the learning phase … this is recall!!! It’s exhausting. Now I just say HEY! with exuberance and don’t even bother trying to remember their name.
The challenge with pulling out words from my memory is not just about names. In conversations I often can’t grab onto the word that I want, when I want it. I feel like I have to walk through all of the Get Smart doors before I can access a huge portion of my vocabulary. Pisses me off because I’m a fast talker and it affects my witty repartee.
The transfer of info into my long term memory doesn’t appear to be functioning.
As I say – I’ve never been a rock star at learning names. It’s always taken a long time. Rehearsal has always helped. I would say a new name a few times in the conversation and bingo! Nailed it.
Now, on the other hand, I can hold a name in my short term memory for about 5 seconds but it doesn’t get transferred into my long term memory. Going to a new school with almost 500 kids is kicking my ass!! A student will tell me their name and as they look up at me, smiling broadly, in my mind I’m thinking “Hi xx. I’m really sorry but it’s going to take me about a year to remember your name. Just tell me it EVERY TIME we meet.” I’ve been at my new school 4x and can remember one kid’s name, and that’s because we had a meeting with the kid’s parents. (Ok two kids, but I knew the other kid before I went there.) I figure I either initiate school uniforms with names on the chest or have a kid walk with me and be my name person. I could point to a human or say a clue like “red shirt”, and they would say their name. Seems easy and effective. And if I spread it out, no one would really miss a whole lot of their education.
My working memory has a short time limit.
Note: working memory is a part of short term memory.
For example, the other day I was meeting with someone to talk about an important issue. While I was listening I was doing what we all do in meetings: processing the information, making connections to other things I knew about that thing, asking questions in my head, identifying the main ideas (and jotting them down), making judgements, a plan of action (e.g., “ok, I need to be sure to xxx”). As if that wasn’t enough, at some point in the conversation I was also thinking “oh crap that reminds me, when this person takes a freaking breath or wraps it up, I’m going to need to ask them about xx”. Blah blah blah and eventually the conversation wrapped up. I was then ready to shift to the other idea / topic / important thing. But you guessed it, that idea / topic / important thing was LONG GONE. There was ZERO chance that I would EVER remember. ZERO. (Making a note right now: buy more sticky notes.)
I miss my working memory. Now when I’m in the veggie section of the grocery store and think “oh didn’t put sour cream on the list – I must grab some”, I head there immediately or kiss the sour cream goodbye. No list? No hope.
What can I do to mitigate it?
I had an appointment with my oncologist yesterday and described the memory issues I’m having. She said that it was normal and it’s early days yet – plus the major coronary event will have added to that. (Waa?? Hmm.) I asked her what kinds of mental exercises I can be doing to help me kickstart my brain. She said “I guess you can look it up online.”
THANKS. A. LOT.
The only advice a cancer patient EVER seems to get from an oncologist about recovery is to: get plenty of rest, eat healthy foods and exercise. Blah. Blah. Blah. No. Fucking. Kidding. It’s as if they are programmed for providing treatment to kill the disease, but not to aid in the recovery. You’re on your own. Just eat more veggies. That should help.
So today at treatment I mentioned something about it to my nurse (to be honest I totally forget what I said LMAO). She brought me a much photocopied booklet called “What you can do about Cancer-Related Cognitive Dysfunction”. Bingo! Several logical strategies about organizing yourself, but also some good strategies under “How can I sharpen my mental ability?” Love the avoid multitasking suggestion. I’ll get right on that. Hahahahahaha
Note: I was able to find a more up to date version of this booklet online.
How long will it go on for?
I’ve been told 3 months to 1 year. Other research says that it takes rats 3 months to regain their memory which translates to 10 years for me. Great.
Next time you come over, wear a name tag.



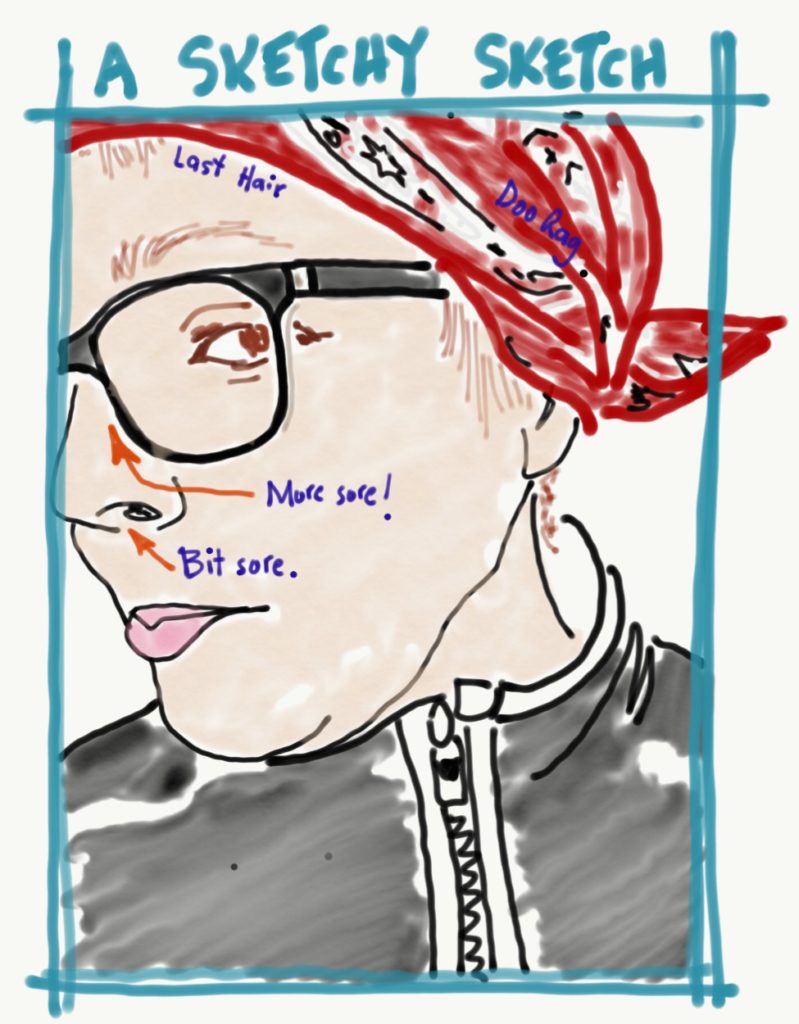
 I had my head shaved last week, on week 9 of chemo. (My hair actually lasted a LONG time!) I had it shaved since it was looking a bit Donald Trumpish. It really did look pretty horrible – my scalp was very visible and the remaining hair was wispy and elfin. I could stand it up and look like a troll. (kind of fun…) And my wigs would just float around on top of my head. (very irritating) So I went with the kids to Jenny’s shop in Lakefield and we all had haircuts.
I had my head shaved last week, on week 9 of chemo. (My hair actually lasted a LONG time!) I had it shaved since it was looking a bit Donald Trumpish. It really did look pretty horrible – my scalp was very visible and the remaining hair was wispy and elfin. I could stand it up and look like a troll. (kind of fun…) And my wigs would just float around on top of my head. (very irritating) So I went with the kids to Jenny’s shop in Lakefield and we all had haircuts.