These days I’m thinking about being DONE and what it means for me to be DONE (yell a bit when I put done in caps, ok?).
I’ll break it down a bit for you. In the next two weeks I have:
- a meeting with my surgeon
- my final Herceptin treatment
- my portacath removed
Each of these appointments represent a different kind of DONE (nice job) and a bit WOOT WOOT (emphasis here too, please, maybe twist your wrists in a circle).
Surgeon Visit
First of all, surgeon man is very charming WOOT WOOT, so I like to visit him, and this will be my last visit with him. Nuff said about that. Secondly, I’m planning to talk to him about plastic surgery and the hypothetical referral that I was given by someone that I cannot recall right now (I think it was he the surgeon, but could have been my family doc). Bottom line is since I don’t know who said they’d refer me, or who they said they’d refer me to, I haven’t been able to follow up, and therefore I don’t know where I’m at with the referral. This is my life. Just ask my secretarial staff.
I digress. Why do I want a referral? Two reasons:
- My chest wall looks like sand dunes. I don’t need breasts, but I’d prefer tabla rasa rather than a Dali-esque distorted chest wall. Who cares, you might ask? Well, I care. When I wear clothes that cling I don’t care that I’m “flat chested / non-breasted” (the name of my imaginary post-retirement company that sells bathing suits with no cups). But I don’t want clinging tops that show the deep tracts of my scars. That just looks wrong. Troughs across my chest are not a great look.
- I want to have some tatoo work done on my chest WOOT WOOT and I’m thinking that the “memories of boob” bumps could impact the design options. (But what do I know about the effects of bumps on tatoos…)

So ya, I want to see a plastic surgeon. Can she (yes, she’s a she, I remember that much), … can she do something easy to flatten me out? What about the one deep sink hole? That thing is just going to look worse as the years pass, I can tell you that.

You can see why the surgeon appointment is an important DONE for me – because it’s a done with a twist. Done with him, and on to surgeon #2. WOOT WOOT!
Final Treatment
This one is a clear DONE. My treatment regimen was 12 chemo treatments (in a row, so once/week for 12 weeks) and 18 Herceptin treatments (once every 3 weeks for a year). I had to miss one Herceptin treatment because of the heart attack, so that’s why I’m finishing 3 weeks later than prescribed. No biggie.
I’ve been counting down the treatments since the summer, each time taking the nurses the same number of treats as treatments that I have left. So it’s become a bit of a “thing” for me. I started with 13 dipped oreos, then 12 muffins …

I really love the nurses in the chemo suite – they’re all so welcoming, positive, gentle, nice… (even the one who I had some reservations about once – I’ve kept my eye on her). Because of the nurses, the chemo suite becomes a safe place to be when you’re in treatment. People are in various stages of feeling shitty, and the nurses treat their patients like family. It’s a nice, calm place to be, and I actually enjoy going. I know that sounds whack, but it’s true. Warm blankets, understanding and a couple of cookies go a long way.
I can’t say that I’ll actually miss going, but it does feel kind of like the end of summer camp. I have to say goodbye. To make it easier, and to thank them for getting me through it, my good friend Annie is coming with me and bringing a whole bunch of her gorgeous charms that she makes out of recycled glass. I’m going to have each nurse choose a charm for her necklace or bracelet. I’m excited to say thank you that way. I think they’ll love Annie’s work. WOOT WOOT!

Truly though, I won’t feel truly DONE till …
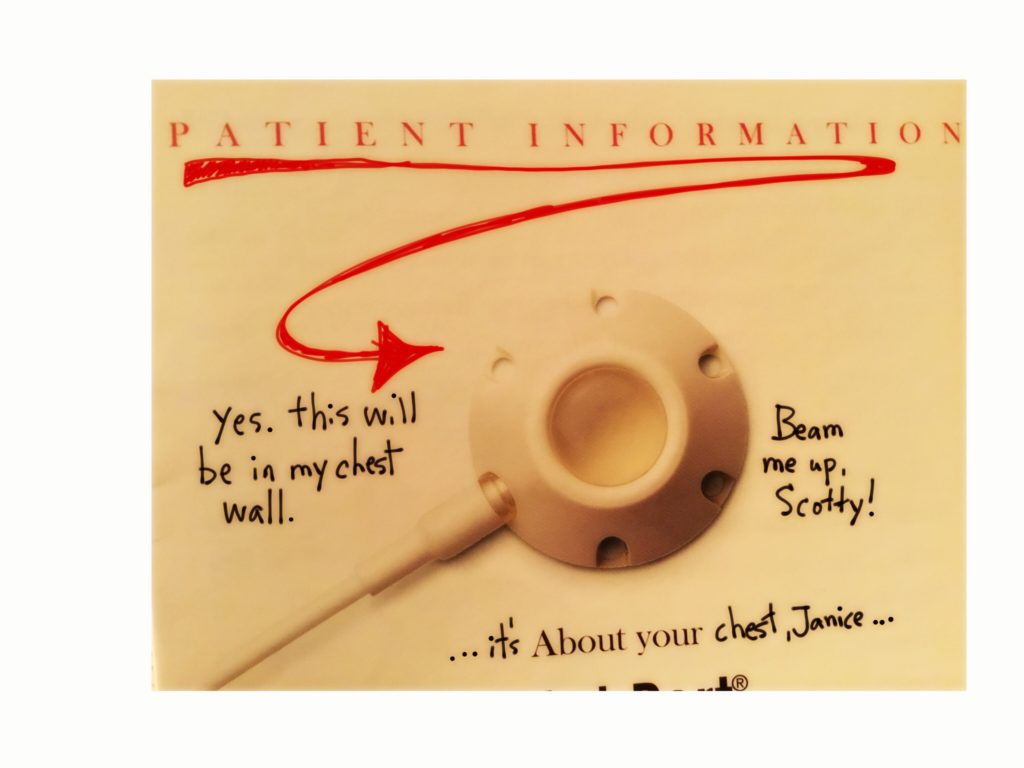
Portacath Removal
I get this sucker out one week after my last treatment. Take a look at this video – it gives me video envy! I have no idea how that woman got permission to video the removal of her portacath, but I’m seriously jealous!! It’s so cool to be able to see what’s being done to you.
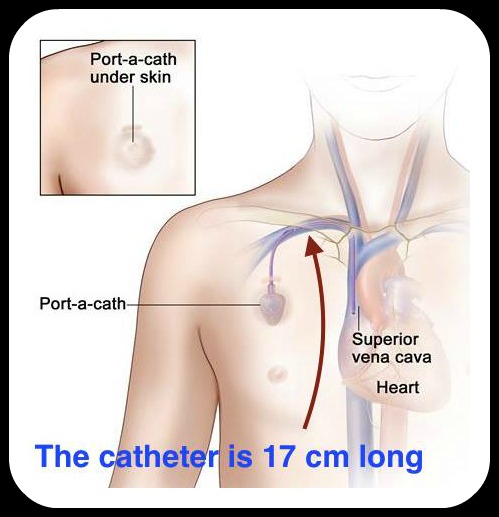
Having the portacath has been a huge asset. It has been so easy for the nurses to deliver chemo and Herceptin. I have seen some of the other patients’ struggles with collapsed veins, and I’ve felt so grateful for my port. It was also super handy when I had morphine injected straight to my heart while I was passing that GD kidney stone! The relief was literally INSTANT (jazz hands here).
Many people will tell you that cancer is a “journey”. It’s true, it is. My journey is almost DONE. It’s about fucking time.