Here is diagnostic imaging. More times than not there is no one sitting at the desk. Thus the bell. I cannot figure that out. I mean, why not sit at the desk? Why sit behind the door and wait for someone to ring a bell? Strange. But I digress.

Why Here?
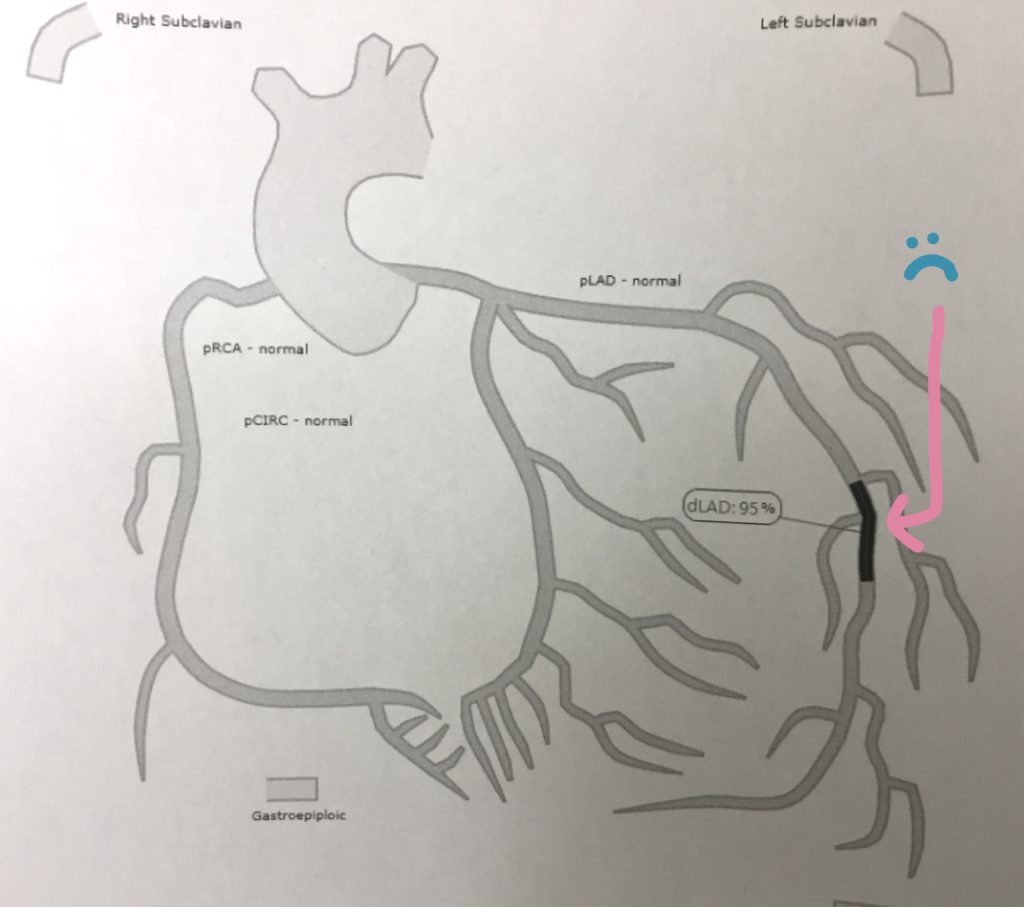
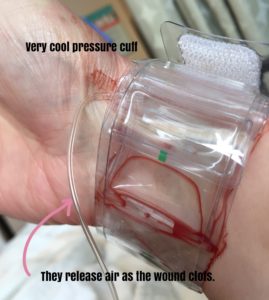
This is the area where I get my MUGA scan done. This is my 4th MUGA. And I’ve had other tests done in diagnostic imaging too – I had my port put in here. Had a couple of CT scans of my carotid and renal arteries after the heart attack. An MRI after the initial breast biopsy to help them determine how much of my boobs they’d chop off. An angiogram to figure out why I had the heart attack. That’s all I think. (You could also have a bone density tests, x-ray, ultrasound – oops had one of those when I was passing a kidney stone. Forgot about that one. But there are a lot more tests there and I am not having them.)
This is the volunteer guy who walks people to the correct room. Why? Because it’s a freaking labyrinth. (You’ll note he’s walking away from me. I know my way.)

The MUGA
First of all the guy who does the test is not a nurse. He’s a nuclear medicine technologist and he is one of my favs at PRHC (other than you Jen). He is super friendly and reminds me of Brent Butt. Spitting image. But all business and not very funny. Ok not funny at all.

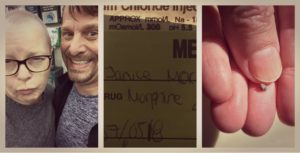
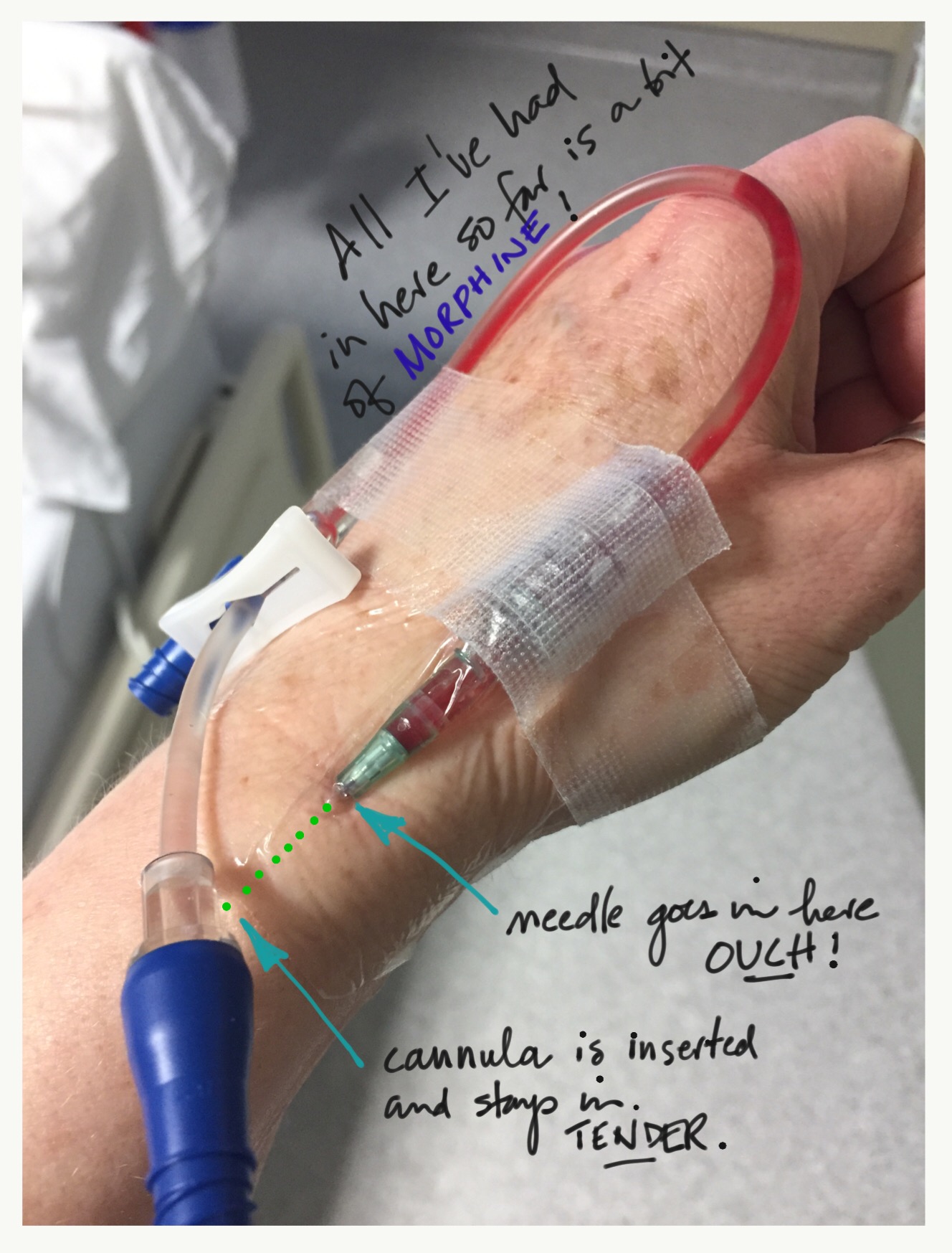
MUGA stands for multiple gated acquisition. (Huh? Don’t worry about it. Keep reading and you might see that there are some gates. Or you might not.) Getting the MUGA is a three-step process. You get the first injection (needle) in a little office.

The stuff in the first injection is a tracer. It essentially helps the radioactive stuff in the second injection stick to your red blood cells. You have to wait 15 minutes after the first injection, then Brent will come and take you to the machine where you get your second injection. (You’re not allowed to take pictures of all this stuff so my photography had to be done skillfully and without Brent noticing. Heh heh.)
Setting up for the Test
The second injection happens JUST before the test and that is done in a big expensive machine called a gamma camera. There are 2 at the PRHC.

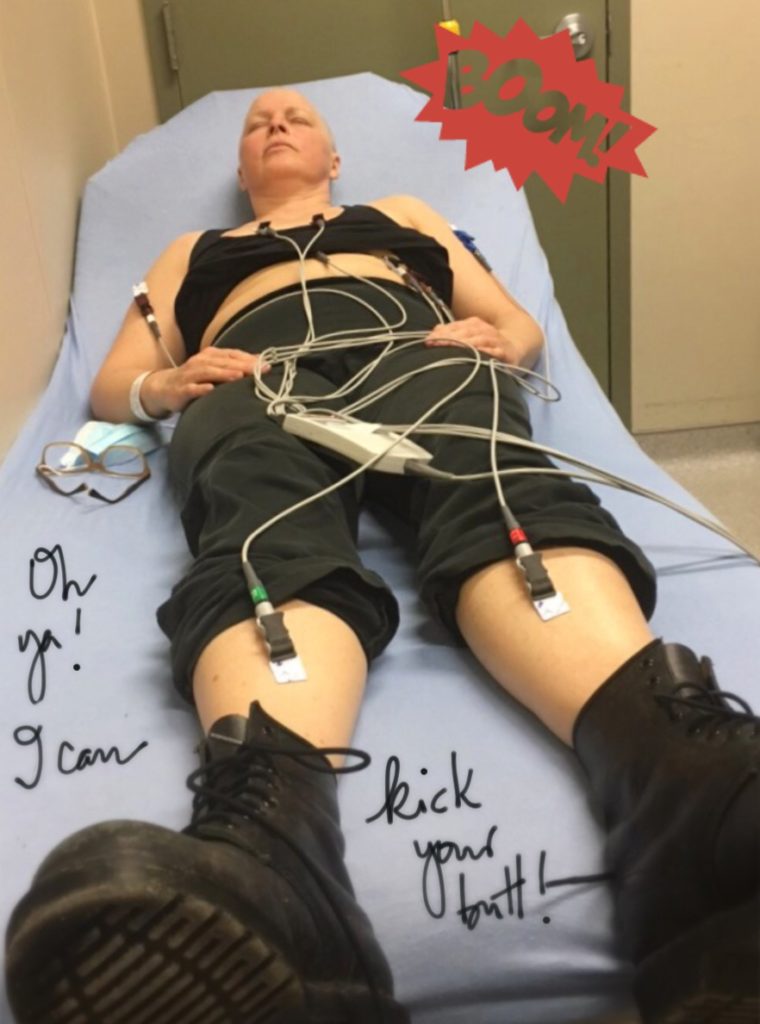
The remainder of the MUGA prep happens on the very narrow but relatively comfy million dollar bed:
- 2 sticky electrodes are put on my chest and 1 on my side (clothing choices matter, people!)
- 3 leads (long wires) are hooked up to the pads (to measure the heartbeats)
- Brent gives me the 2nd needle, this one full of radionuclide with a half life of 6 hours (honestly the radioactive stuff is set up on a little table in such as way that you feel like you’re in the Princess Bride and about to be stretched or given a secret potion)
- I have to put my left hand under my head and my right hand under my butt which feels comfy for the first minute or two
- BRENT covers me with a blanket (not warmed – meh) and the bed slides into the big camera
- the plates lower over me until its about 5cm away from my chest
- the lights dim and I am instructed to lay still and not to fall asleep (slows your heart)
- I lay there for 10 min listening to 80s music and trying not to swallow, sneeze, move or think about the fact that my left shoulder is slowly popping out of my skeleton
- the room is cold because the machines give off a lot of heat … I’m thankful for the blanket and for the triangle wedge under my knees – I think about how nice that would be when you lay in savasana …anything to avoid thinking about the searing pain in my left shoulder
- finally get to reposition after 10 min – now both hands have to go under the butt
- lay still for 10 more minutes and chill out to Genesis and Glass Tiger
Why do I even have this test?
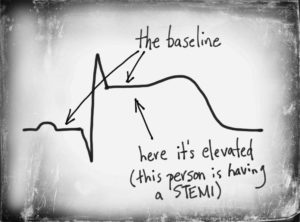
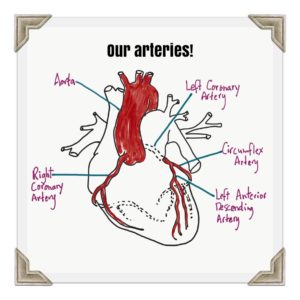
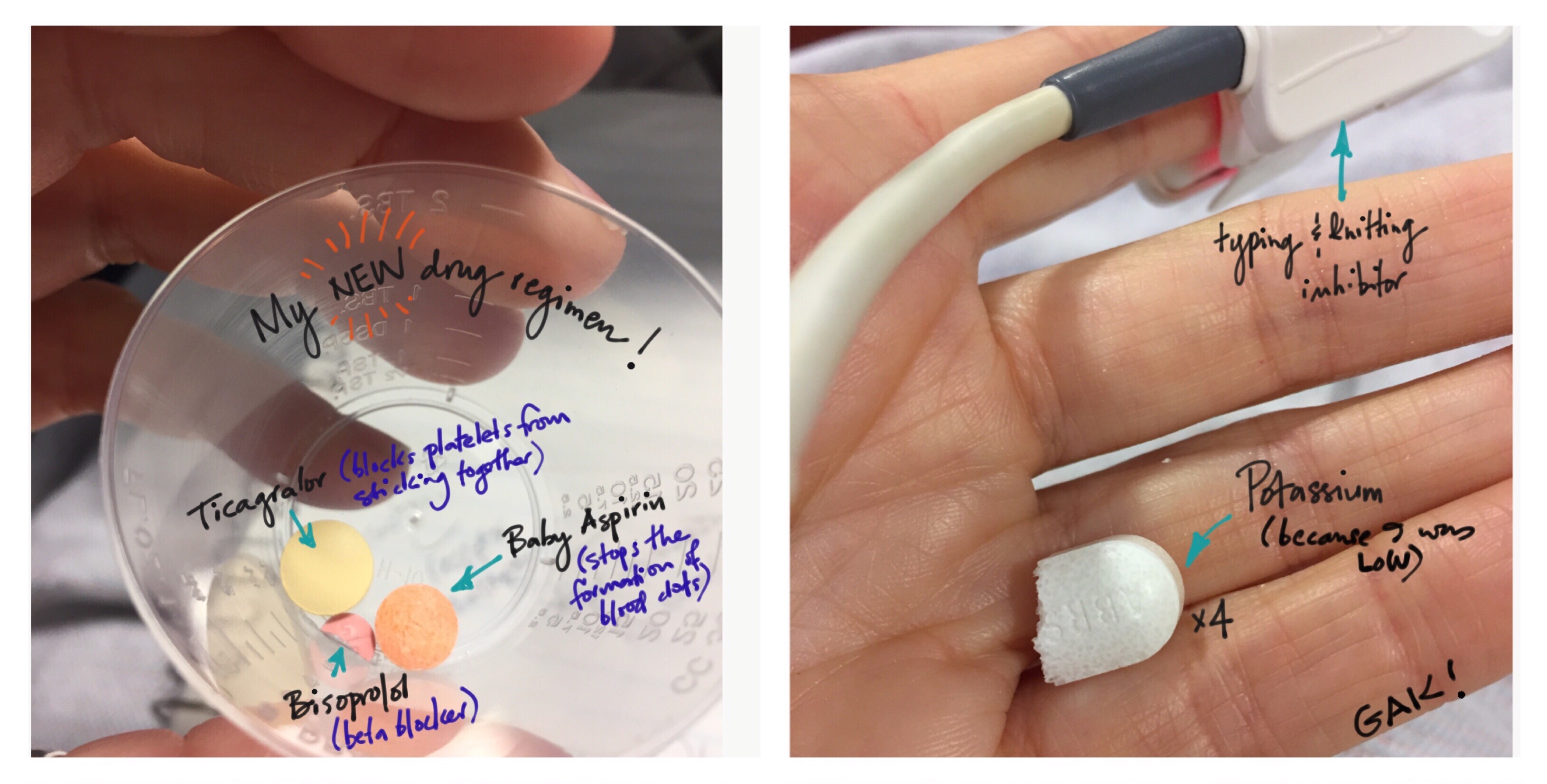
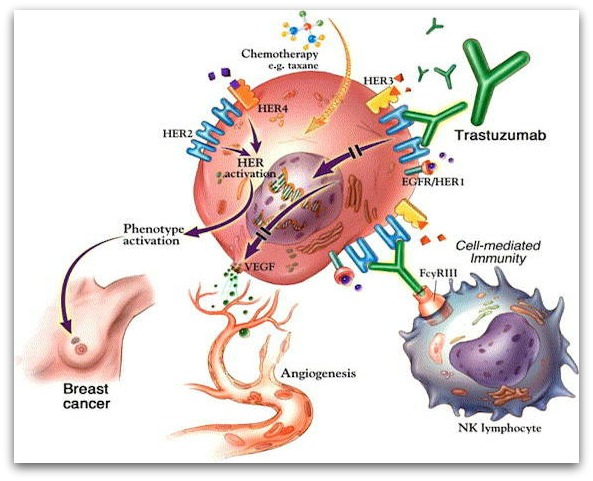
Brent explains that the scan itself is essentially a movie of the heart beating. They are measuring the strength of the muscle as well as the “ejection fraction” or the rate at which the heart is pumping the blood out. If the scores drop then my oncologist re-evaluates my treatment because one of the major side effects of Herceptin, the treatment I’m getting for my HER-2 positive breast cancer, is that it can be pretty hard on the heart. (But the heart attack was TOTALLY UNRELATED.)
Ta ta to Brent – I’ll see him in another 9 weeks for MUGA #5.